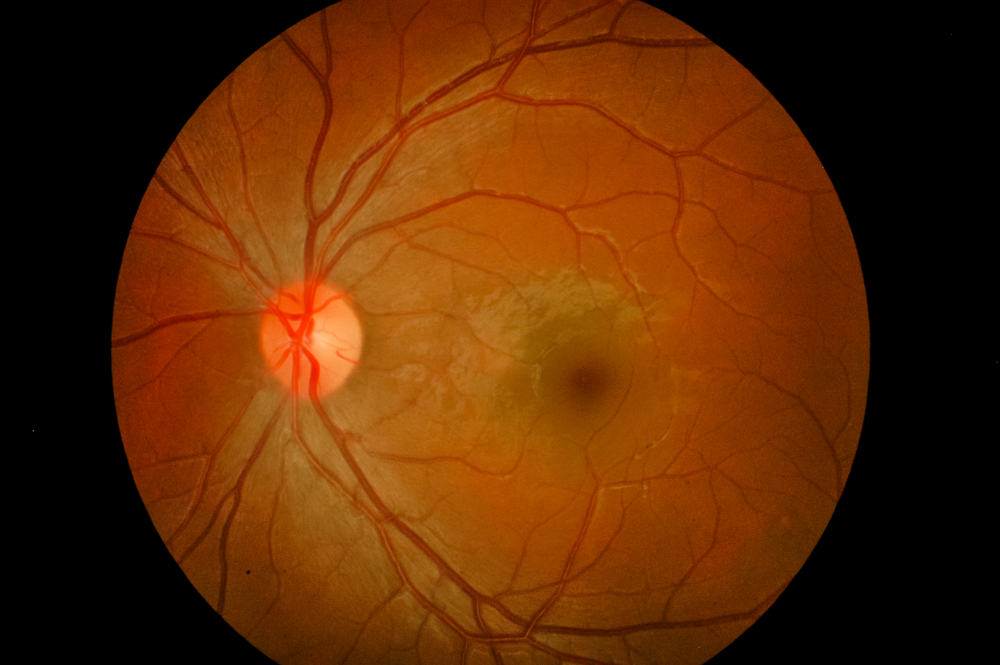
Age-related macular degeneration affects more than 200 million people worldwide. A distinction can be made between dry and wet AMD, with the dry form making up the majority of patients, while wet AMD is considered more aggressive and leads to severe visual impairments. An early symptom is blurred vision, where straight lines appear distorted. This can result in darkness, whiteouts, or blurred areas in the center of the field of view. AMD is one of the leading causes of irreversible blindness worldwide. Although some therapies delay central vision loss, no current treatment completely restores it.
Abnormal Vascular Growth in the Eye can Lead to Age-Related Macular Degeneration
Scientists from the University of Virginia Health System have identified a new target to prevent the formation of abnormal tangles of blood vessels associated with eye diseases such as neovascular age-related macular degeneration, proliferative diabetic retinopathy and ischemia.
The study has opened up the possibility of mitigating abnormal blood vessel growth in eye diseases by targeting the epigenetic machinery. By locally targeting the epigenetic regulator, researchers have gained a deeper understanding of how ocular immune cells can cause a loss of control over blood vessel growth under the retina. This approach also provides new direction for the development of more effective, less expensive interventions, thereby avoiding issues such as drug resistance, which are a growing problem with traditional anti-VEGF therapies used in clinical treatments.

Scientists already knew that abnormal vessel growth in the eye is fueled by excessive amounts of a substance called vascular endothelial growth factor A, or VEGF, which plays an important role in blood vessel formation. The new research identifies a key protein that determines VEGF levels. Blocking this protein in laboratory mice significantly lowered their VEGF levels in a targeted manner, without any unwanted side effects. For example, the scientists found that it has no toxic effects on the retina, the light-sensitive part of the eye where vascular proliferation occurs. This discovery answers a long-standing question about how ocular immune cells such as macrophages contribute to the abnormal growth of blood vessels under the retina.
In addition to identifying a promising target for the development of new treatments for vision loss, the discovery sheds important light on the fundamental mechanisms responsible for the blood vessel overgrowth that blinds millions of people. While much more research and testing will be needed before the new findings can be translated into a treatment, scientists are excited about the potential of the discovery.
The Role of Immune Cells in the Development of Age-Related Macular Degeneration
When we age, the immune system ages too. Previously, scientists at Washington University School of Medicine in St. Louis found that aging immune cells increase the risk of age-related macular degeneration, a leading cause of blindness. Studying mice and cells from patients, the researchers found that immune cells called macrophages age and are more likely to contribute to the inflammation and abnormal blood vessel growth that damages vision in macular degeneration. Their findings were published in the journal JCI Insight.
In experiments on mice, the team found that older macrophages carry larger amounts of short snippets of genetic material called microRNAs, which control how cells express genes. The researchers found significantly higher levels of microRNA-150 in macrophages in the eyes of older mice. MicroRNAs help regulate many things in cells by binding to multiple genes to affect how those genes make proteins. In this study, the researchers found that in a mouse model of macular degeneration, microRNA-150 appeared to direct older macrophages to promote inflammation and abnormal blood vessel formation. The researchers also tested blood samples from people with and without macular degeneration. Samples from patients with macular degeneration also had significantly higher levels of microRNA-150 in their macrophages.
Macular degeneration therapies are aimed at treating the symptoms of the disease rather than treating the cause. By understanding what happens to the immune cells in the eye, it may be possible to develop therapies to help patients who cannot be helped with existing drugs. If one can somehow reduce microRNA levels in macrophages or alter one or more molecular pathways that are regulated by this microRNA, one could potentially reduce inflammation and disrupt the abnormal growth of blood vessels in the eye.
Certain Protein Plays Key Role in Many Age-Related Diseases
Research published in the Physical Journal suggests that a key protein in the blood is involved in causing macular degeneration and other age-related diseases like Alzheimer’s and atherosclerosis. There are hundreds of proteins in our blood, but researchers focused on vitronectin, one of the most abundant. Vitronectin not only circulates in high concentrations in the blood, but also in the scaffolding between cells and is also a significant component of cholesterol. This protein is an important target for macular degeneration because it accumulates at the back of the eye and leads to vision loss. Similar deposits occur in the brain in Alzheimer’s disease and in the arteries in atherosclerosis.
Through detailed biochemical analysis, the researchers found that the protein can subtly change shape under pressure. These changes cause it to more easily bind to calcium ions in the blood, which the researchers believe leads to the formation of calcified plaque deposits that are characteristic of macular degeneration and other age-related diseases. These structural insights will streamline the development of treatments for macular degeneration by allowing researchers to custom design antibodies that selectively block the protein’s calcium binding without interfering with its other important functions in the body.
Obesity can Cause Age-Related Macular Degeneration
A Canadian study published in the journal Science uncovers another molecular mechanism that can trigger age-related macular degeneration (AMD). Research at Hôpital Maisonneuve-Rosement in Montreal shows how life stressors like obesity reprogram immune system cells, making them eye-destructive as we age.
It is already known that the immune system in the eye of a person with AMD becomes dysregulated and aggressive. Normally, immune cells keep the eye healthy, but exposure to pathogens such as bacteria and viruses can damage them. At the same time, immune cells are also activated when the body is exposed to stressors, such as excess fat in obesity, making obesity the number one non-genetic risk factor for developing AMD.
In their study, the researchers used obesity as a model to accelerate and exaggerate the stressors the body experiences throughout life. They found that transient obesity, or a history of obesity, leads to persistent changes in DNA architecture within immune cells, making them more vulnerable to produce inflammatory molecules. These results provide important information about the biology of the immune cells that cause AMD and could enable the development of more tailored treatments in the future.